Now that we have 4 months of PDPM under our belts, there is enough data available to perform a checkup. Medicare rates are generally higher around the country, but is that the case at your SNF? Even if your average rates are up, Administrators still need to dig deeper to see if the team is functioning at its highest when it comes to capturing PDPM reimbursement and implementing PDPM concepts into practice.
Are you ready for your PDPM Checkup?
1. Break PDPM into pieces. Begin by breaking down your average reimbursement rates for each of the PDPM components (PT/OT, Speech, Nursing, NTA). Is the NTA component higher than anticipated? Is nursing lower than expected? What would your rates be without the NTA component? What are the costs associated with the NTAs that you are capturing? Each component must be accurate and optimal.
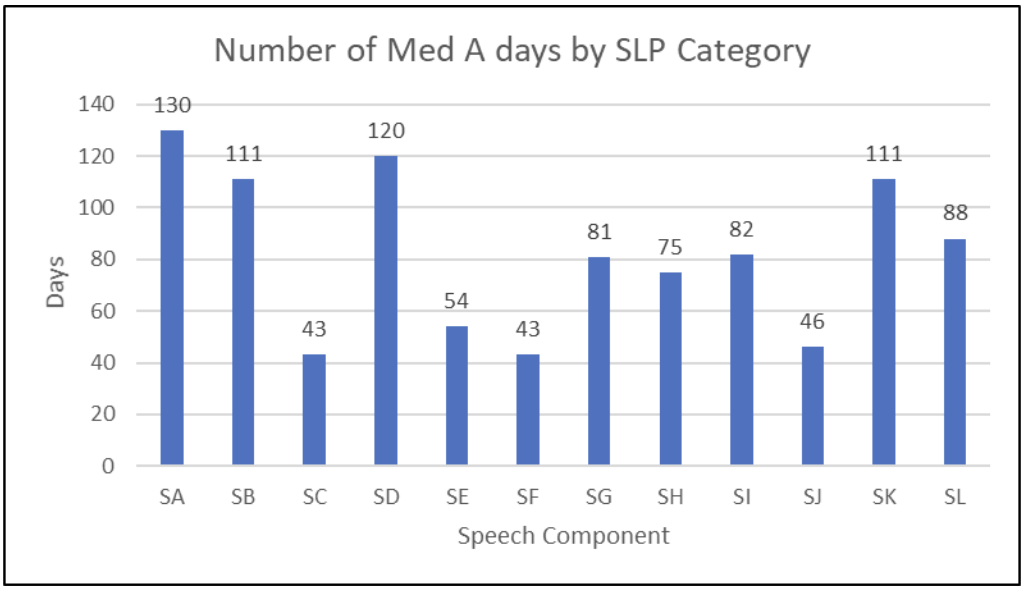
2. SLP Component. The PDPM SLP component has the widest dollar variation from top to bottom. Is the team clear on the parameters coding altered diets and speech-related comorbidities? There is also a heightened importance of accurately coding severe cognitive impairment on the BIMS. Below is a graph of Medicare Days by SLP code from a SNF with a strong speech program and robust Medicare census.
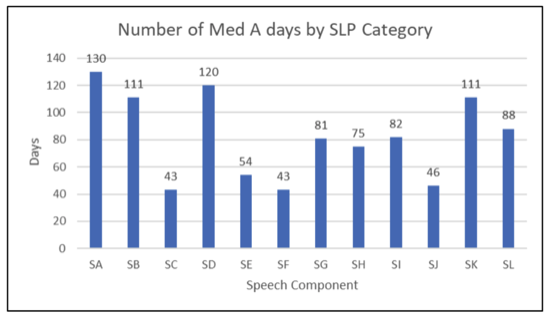
A graph of SLP Component Days
In this region, the reimbursement for a patient coded at “SA” (no speech needs, cognitive impairment, or neuro issues) is $18.56 per day.
Meanwhile, a patient coded at “SL” (neuro diagnosis, swallowing problems, altered diet, cognitive impairment, and speech comorbidities) is $114.94 per day over the entire LOS.
While you can see, most patients fall someplace in the middle, the accuracy of coding by the nursing home speech department is crucial.
Would you like for Language Fundamentals to perform a customized Speech Department Analysis for your SNF? Contact us and we’d be glad to help.