When it comes to evaluating swallowing disorders, selecting the right instrumental exam is crucial. Two primary methods are Fiberoptic Endoscopic Evaluation of Swallowing (FEES) and Modified Barium Swallow Study (MBSS). Both have strengths, making them valuable tools in different situations. Here’s a quick guide to help you decide which test best suits your patient’s needs.
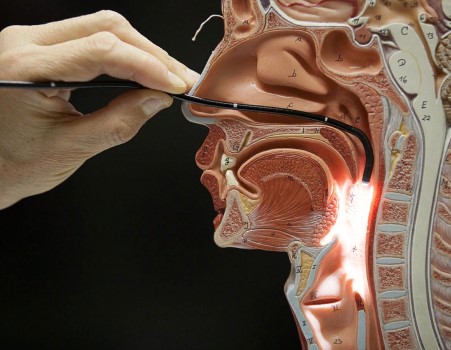
Fiberoptic Endoscopic Evaluation of Swallowing (FEES)
Description: FEES uses a flexible endoscope inserted through the nose to get a close-up view of the pharynx and larynx during swallowing.
Pros:
- Up-Close Look: FEES gives a detailed view of the aerodigestive structures in the throat, helping you assess the integrity of the anatomy and see exactly what’s happening during the swallow.
- Real-Time Insights: Watch how your patient manages secretions and see the effects of fatigue over time.
- No Radiation Worries: Safe for repeated use without concerns about radiation exposure.
- Bedside Convenience: Can be performed right at the patient’s bedside, perfect for those with mobility issues.
- Cost-Effective: Generally, less expensive than MBSS and doesn’t need a radiology suite.
- Familiar Faces: The primary SLP is actively involved, ensuring continuity of care.
Cons:
- Partial View: Can’t visualize the oral or esophageal phases.
- Temporary Obscurity: The view is momentarily blocked during swallowing.
- Nasal Discomfort: Some patients may find nasal insertion uncomfortable.
- Increased Special Training Needed: Requires significant training and experience to utilize the endoscope and interpret images accurately.
Modified Barium Swallow Study (MBSS)
Description: MBSS, or videofluoroscopic swallow study (VFSS), involves the patient swallowing barium-coated food while X-ray video captures the swallowing process from start to finish.
Pros:
- Comprehensive Overview: Provides a full view of the swallowing process, including oral, pharyngeal, and esophageal phases.
- Detailed Diagnostics: Identifies aspiration, penetration, and bolus transit issues throughout the swallow.
- Structural Clarity: Reveals structural abnormalities like diverticula or strictures.
- Clear Measures: Offers precise data on swallowing efficiency and timing.
Cons:
- Radiation Exposure: Limits the frequency of use due to radiation concerns.
- Accessibility: Requires a radiology suite, which most often means an outpatient trip to the hospital.
- Time limits: Typically done quickly to avoid radiation exposure, which might miss issues related to fatigue.
- Higher Costs: More expensive due to radiology services and barium.
- Logistics: Needs additional staff and patient transport to the hospital.
- New Faces: The primary clinician is typically not present, which can affect patient comfort and outcome of endorsed information.
Both FEES and MBSS are fantastic tools, each with its own set of strengths. If you need a detailed, real-time view of the pharyngeal and laryngeal structures, and your patient could benefit from a portable, radiation-free test, FEES is an excellent choice. On the other hand, if a comprehensive overview of the esophageal phase is crucial, and you need to identify specific structural abnormalities, MBSS might be the better option, despite its higher cost and radiation exposure.
Ultimately, the choice depends on your patient’s specific needs and the resources available. By understanding the pros and cons of each method, you can make an informed decision to ensure the best possible care for your patients.